Supplement 2 - East Lothian's model of health and social care
Report: Changing models of health and social care >
1. Taking a whole-system approach
Read more...
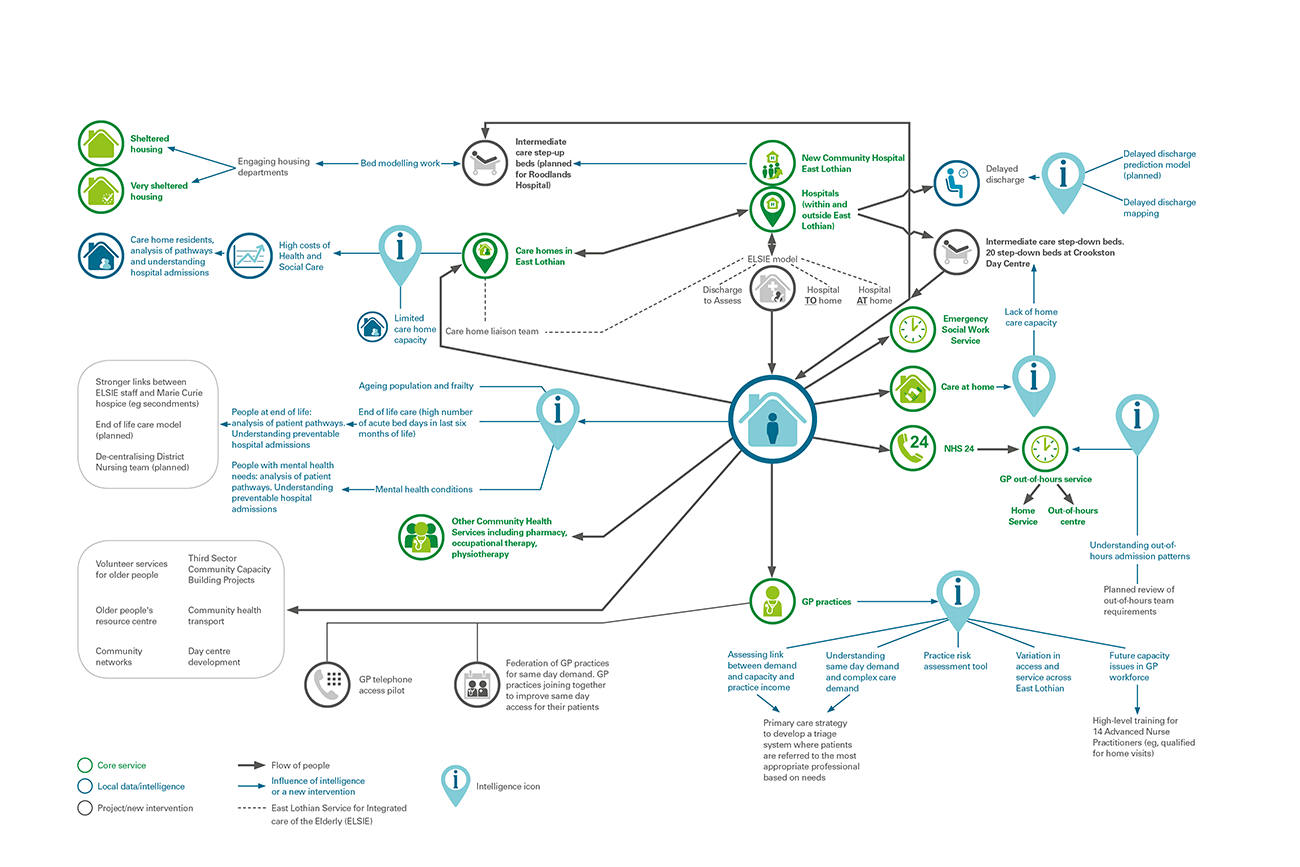
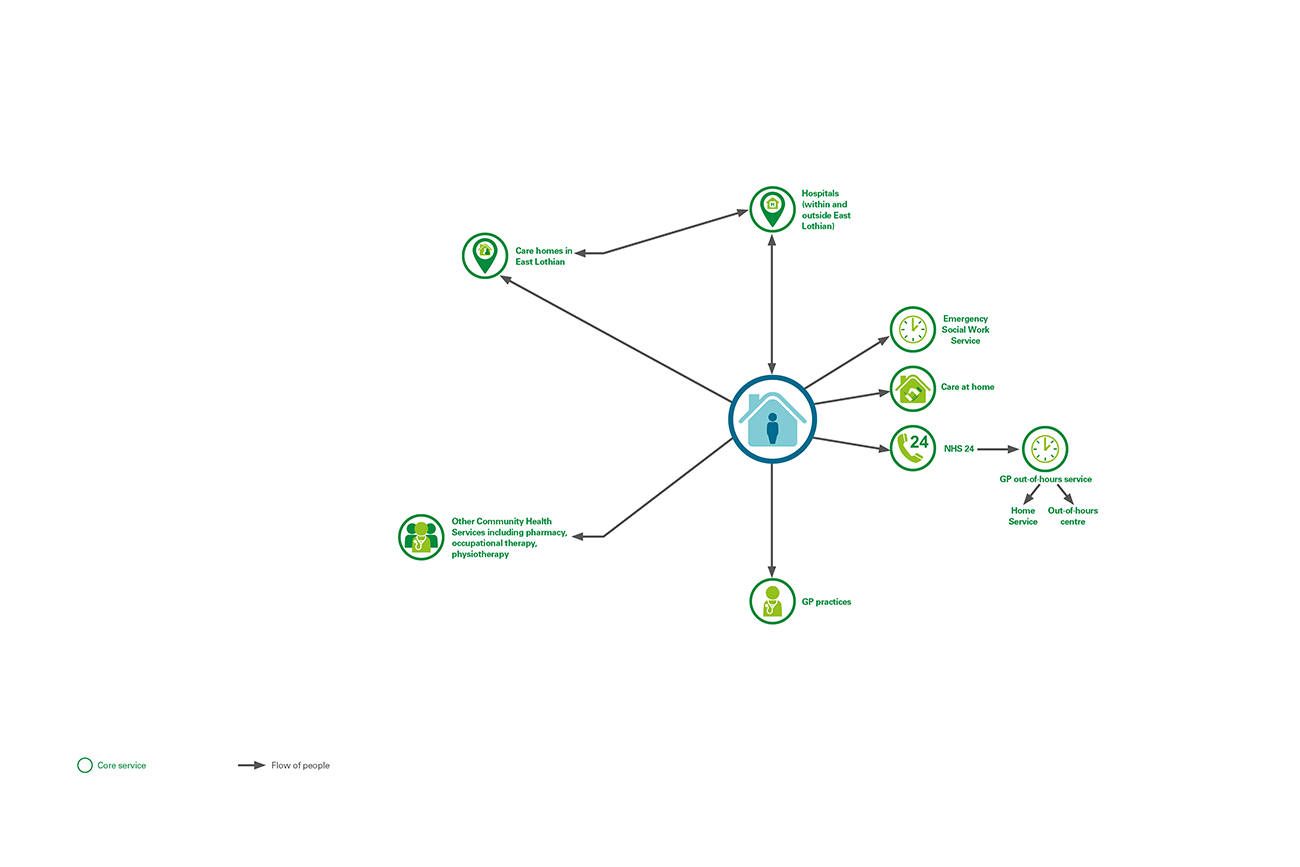
East Lothian is taking a whole-system approach to understanding its local population and planning health and social care services. This involves:
- recognising the inter-dependent nature of the system and that actions in one part of the system may have an impact on the whole system
- increasing capacity in community services to avoid the need for admission to hospital and support earlier hospital discharge
- using existing capacity as efficiently as possible and effective partnership working between hospital and community services, and across health and social care services.
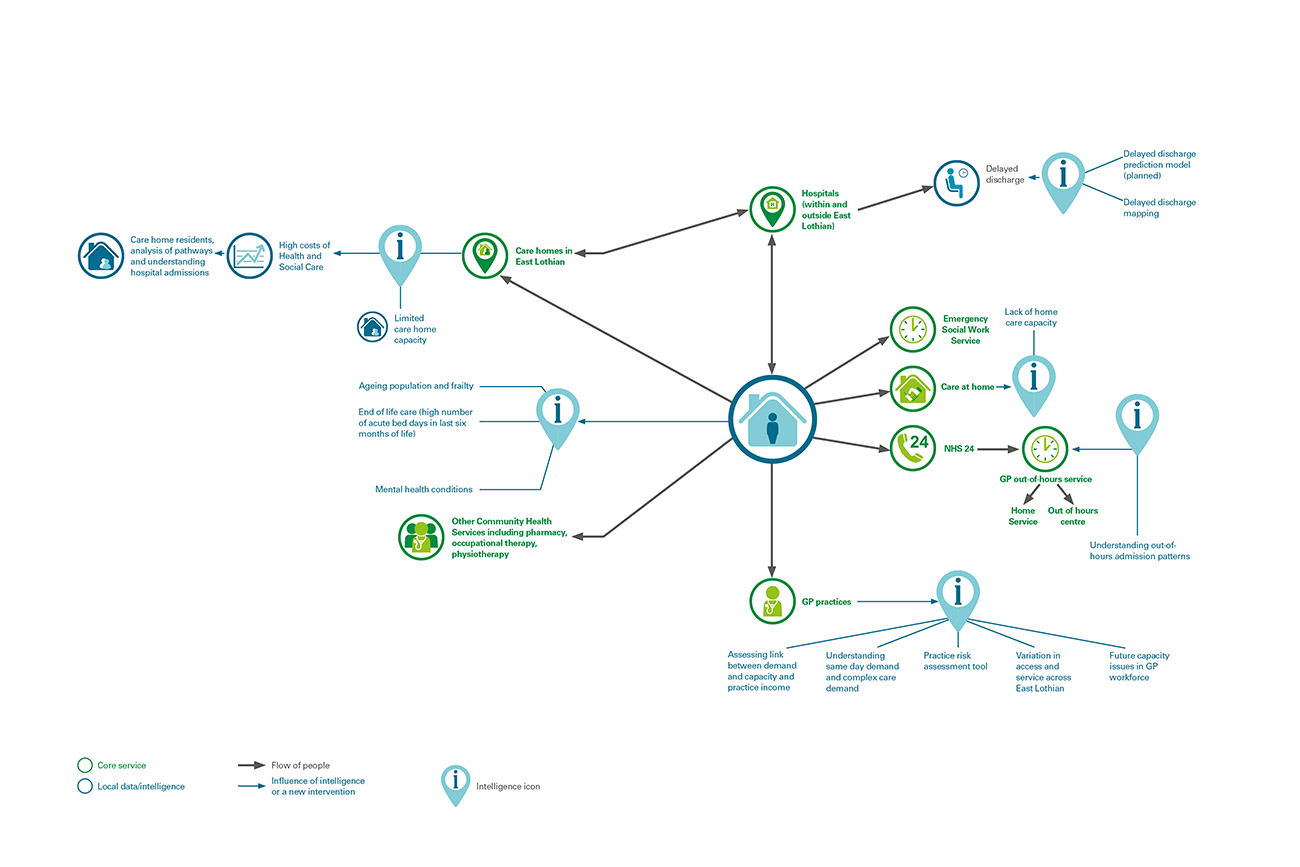
The partnership is using local data and intelligence about its population and services to improve care and outcomes for its local population. It is using a whole-system approach to identify more efficient ways of providing care and aims to support people in the community wherever possible.
2. Key intelligence about the population and services
Read more...
East Lothian is bringing together local data analysis and intelligence about its population, and how people access services, to improve how it delivers services. It is building a comprehensive picture of:
- the needs of its local population,
- the groups of people making most use of services (not to criticise them but to aid understanding of service use), and
- how changes to services affect different parts of the health and social care system.
Analyses show:
- East Lothian has an ageing population with increasing levels of frailty and complex health needs.
- Increasing hospital admissions from younger people with increasing long-term conditions and ill-health in some local areas.
- The groups of people who use a disproportionately high level of health services are those who: are nearing the end of their life, are in care homes or have mental health needs.
- Relatively low numbers of people are being admitted to hospital in an emergency, but with high rates of occupied bed days and delays in discharge from hospital.
- There is a lack of capacity to meet demand for home care.
- There are a number of issues for GPs including a high level of demand for services, a predicted shortage of GPs due to an ageing workforce and variety in the ease of access to GPs in different practices in East Lothian.
3. New services and interventions and 4. Intended impact
Read more...
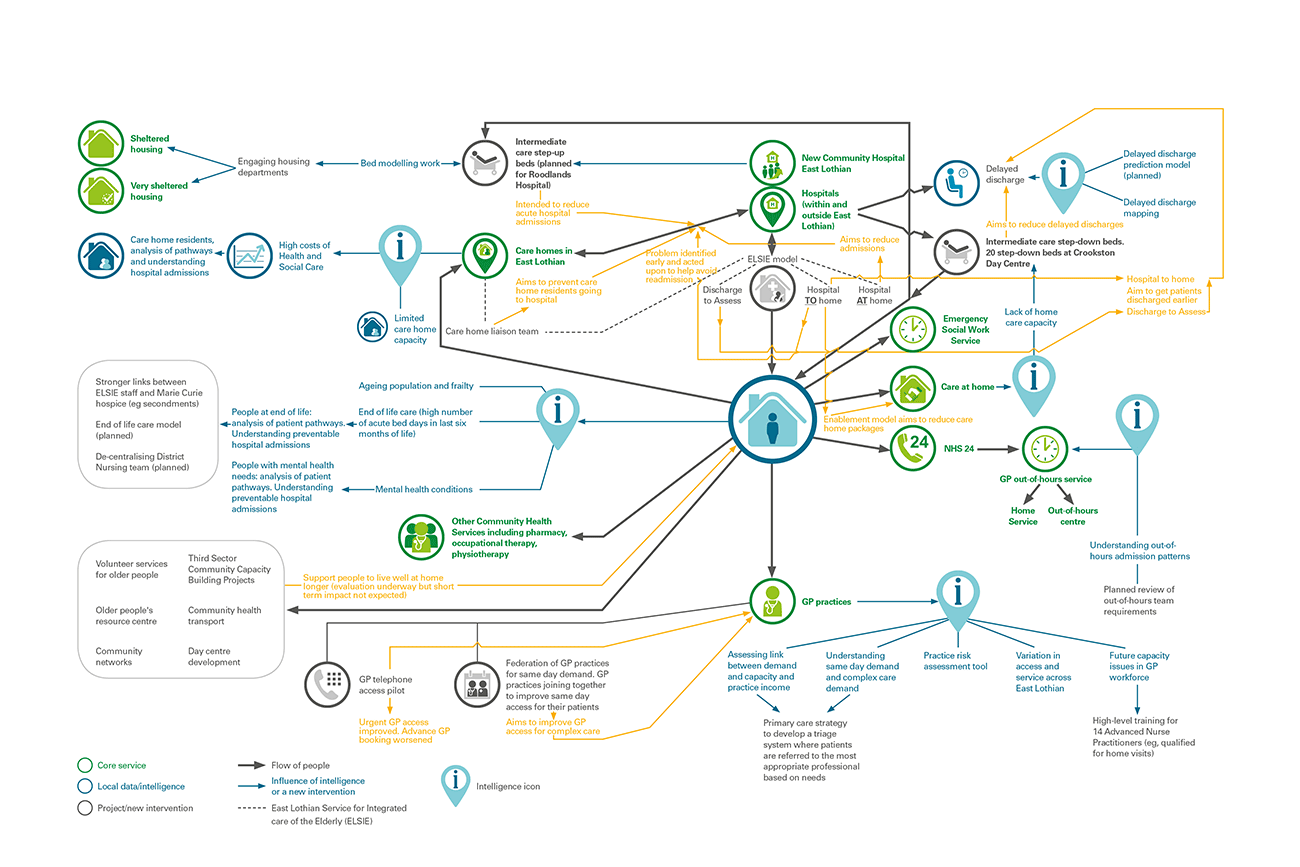
East Lothian is using the intelligence it has gathered to inform the development of a number of new services and interventions:
- East Lothian Service for Integrated care for the Elderly (ELSIE) is a comprehensive and integrated health and social care service for older people delivered by a multi-disciplinary workforce. The impact of ELSIE has still to be fully evaluated. It has a number of key components:
- Hospital at home - a service for critically unwell patients, referred by their GP, who can be cared for in their own homes, or the place they call home, in an acute stage of their illness to prevent admission to hospital. A patient survey and monitoring of patients aged 65 and over is being carried out.
- Hospital to home - facilitates hospital discharge for medically fit patients waiting in hospital for a care package. The team provides a care package until a long-term care provider is found. More analysis is required to assess the impact of this service, but initial findings indicate that it is: reducing length of delay; providing continuity of care that reduces the likelihood of readmission; and reducing the need for care packages by using a reablement approach.
- Discharge to assess - occupational therapists and physiotherapists assess patients at home, allowing them to leave hospital earlier with additional support. The team can provide equipment, ongoing rehabilitation and a package of care on a short-term basis. Patients using this service are being monitored to assess the impact on their length of stay.
- Care home liaison team - provides an education service to support care home staff to provide a hospital at home level of care in a care home setting, for example showing staff how to administer specialist feeding techniques. It is thought that this is preventing care home residents being admitted to hospital, but more evidence is required to confirm this.
- Intermediate care - 20 'Step Down' beds at Crookston Day Centre are available for patients in an acute hospital who require additional time and rehabilitation to recover but are unable to have this provided at home. In the longer term, the plan is to move towards a 'Step Up' model of care at Roodlands Hospital, where patients will be admitted from home instead of being admitted to an acute hospital.
- Community capacity building - a number of third sector projects have been set-up using the Change Fund.
- Advanced Nurse Practitioners - are currently being trained and will be qualified to visit patients at home.
- Total telephone triage pilot - prioritised patients based on their needs and urgency, and offered patients with less complex needs a telephone consultation. The pilot had both a negative and positive impact on patients. During the pilot period it was the only practice in East Lothian to experience a significant improvement for patients requiring urgent access to a doctor or nurse, but a significant reduction in the proportion of patients able to make an appointment with a doctor three or more working days in advance. The practice partners chose not to extend the pilot into normal working practice.
East Lothian plans to carry out a whole-system evaluation of services during 2016. The results of initial analyses have led to East Lothian planning further work to:
- understand the extent to which delayed discharges can be estimated using a predictive model
- analyse the pathways of individuals using high resources in the health and social care system to establish whether preventative models of care could make a difference
- develop an end of life care model
- analyse the different patterns of admissions through out of hours services
- engage with the housing department on the provision of sheltered and 'very sheltered' housing
- understand demand and capacity in primary care in East Lothian and links to general practice income
- use a practice risk assessment tool to assess the risk of individual practices failing as a business or closing.